Congratulations, athletes… now that you’ve hit month 7, you’re officially embarking on the second half of your ACL recovery journey!
Perhaps it doesn’t feel like it warrants much congratulation; for some, it can be more daunting than anything. After all, you’ve been working so hard for so long, yet you’ve still only just gotten past that halfway mark.
And trust us, we know — it can be a lot to think about how much left there is to go.
It may be frustrating to have another six months to work through, but you can imagine how much more devastating it would be to put in half a year’s worth of work only to reinjure yourself after returning to play before you were ready. Most athletes who return after only 6 months of rehab will see a much higher rate of injury (which we’ll explain why in just a second).
So be sure you work through that full year; it’s absolutely vital to come out the other end stronger and 100% ready to get back out onto the field!
Why Does It Take a Full Year to Recover from ACL Surgery?
Perhaps some of your frustrations may dissipate with a bit of extra context. There are multiple facets as to why ACL rehab necessitates an entire year, and we’re here to explain it all for you.
Let’s start with the healing process itself.
As we’ve previously mentioned in this series, when you first undergo surgery, your ACL graft needs about 3 months just to adapt to the environment of your body. (Think about that in the context of a shorter rehabilitation window; if you only rehabilitate for 6 months, your ACL will have only fully healed by the time you’re halfway through that timeline! That’s a huge red flag.)
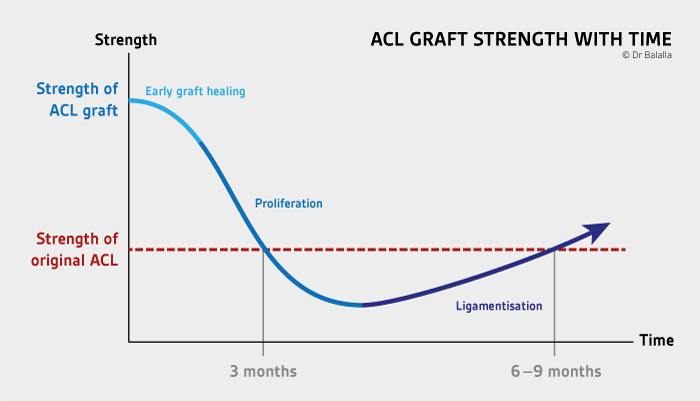
Then take into consideration the amount of muscle atrophy that occurs after surgery: your quadriceps, hamstrings, calves, and glutes are all prone to significant weakness during this initial phase of recovery. And while you can certainly rebuild your strength back up, it doesn’t just happen overnight — most athletes can expect to achieve sufficient muscle strength approximately 6 to 9 months after surgery.
And that’s only the beginning!
In addition to graft healing and normalized strength levels, you’re also going to need significant time for regaining optimal motor control for sport-specific movements at game speed. To pass a comprehensive return-to-sport test, your movement has to be fluid, efficient, powerful, and accurate, all at top speed. (And that’s no easy feat, as we’re sure you’ve learned by now.) Achieving this level of movement mastery typically takes anywhere from 3 to 6 months.
Most athletes start dynamic movement training around months 4 through 6, meaning they’ll likely range around 10 months to a year by the time they’re ready for a proper return to sport.
Physical Therapy During Month 7
By this point in your timeline, you’ll have likely obtained some solid data about your movement strategies and any biomechanical deficiencies. As we mentioned previously, going through this first round of testing is essential for building an optimal rehab program moving forward. (It’s all about addressing your weak links so they’re no longer a detriment to your performance!)
While your rehabilitation plans moving forward will vary from athlete to athlete, there are a handful of common issues that we’ve seen repeatedly through our years of facilitating ACL rehab and RTS results…
Common Issue #1: Pelvic Drop
This is an extremely common form error for many athletes even without having undergone ACL surgery — so, you can imagine why it’d be the same case for those who have.
Pelvic drop is as straightforward as its name suggests: it’s when one side of your pelvis drops lower than the other. Your gluteal muscles are typically responsible for keeping your pelvis level, especially during single-leg activity. And whenever there’s pelvic drop, there are usually compensations in other parts of the body…
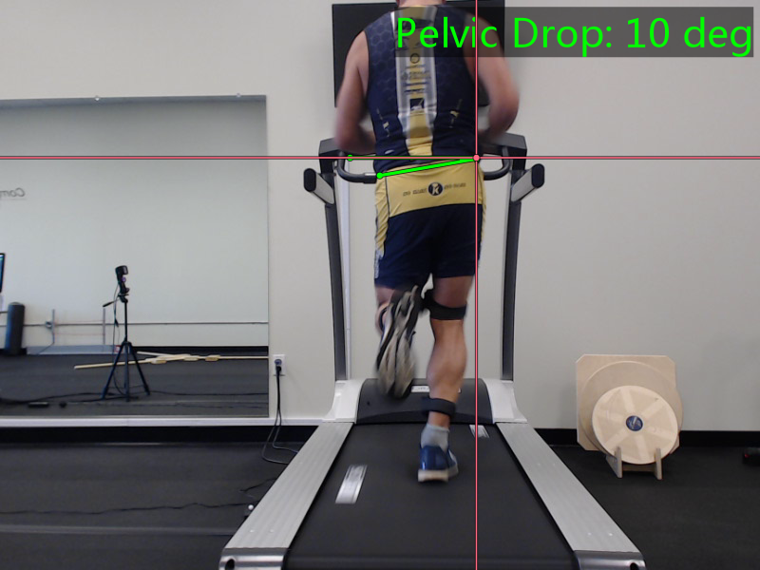
One of the most common compensations is a shift in your trunk lean. When one side of your pelvis drops, your center of mass naturally shifts to the lower side. Your body then starts to lean in the opposite direction to try keep from falling over. (This can then lead to other compensatory issues… but let’s stick to one thing at a time.)
Experiencing pelvic drop doesn’t inherently mean that you haven’t been strengthening your glutes well enough; while it could be an issue of imbalanced gluteal strength, pelvic drop has as much to do with gluteal control as it does strength, making it an extremely common error for just about any single-leg-based movement.
The key to fixing it? Lots and lots of single-leg practice.
Focusing on exercises like step-downs and fast single-leg squats is an excellent means of deliberately practicing pelvic and trunk lean control. Additionally, practicing deceleration is vital to ensuring you’re able to maintain a level pelvis during high speeds and changes of direction.
Common Issue #2: Decreased Shock Absorption
Shock absorption is vital for most physical activity, especially those at game speeds — but your knee plays a key role in effective shock absorption.
More specifically though, it’s the knee bend that makes it happen. We’ve talked about it a little in the previous installments, particularly in the context of safe running; the basic gist is that optimal knee flexion leads to better muscle contraction, and that’s what makes for optimal shock absorption.
So, you can imagine why bending the knee at faster speeds can still be daunting or difficult to commit to. (Heck, you’ve been living it.)
Take this video below. It’s specific to the biomechanics of running, but it provides valuable insight into training single-leg shock absorption:
All this adds up to even more single-leg work! But this time, your exercises are less focused on the balancing act of pelvic control; honing shock absorption requires more plyometric work. Think workouts like single-leg bench squats and single-leg jumping (forward jumps and box jumps).
Having access to a force plate to measure proper forces and shock absorption can be incredibly helpful in this process. Your physical therapist can use the force plate’s data to ensure the readings are equal in both individual legs, ensuring that both extremities are sustaining the same forces.
Common Issue #3: Knee Collapse
This one might seem more predictable (you know, since it directly involves your knees).
Inward collapsing at the knees, also referred to as knee valgus or internal knee rotation, is extremely common as you ease back into sport-specific movements. At this point in your rehabilitation, it’s most prominently seen as you practice 45- and 90-degree cutting drills.
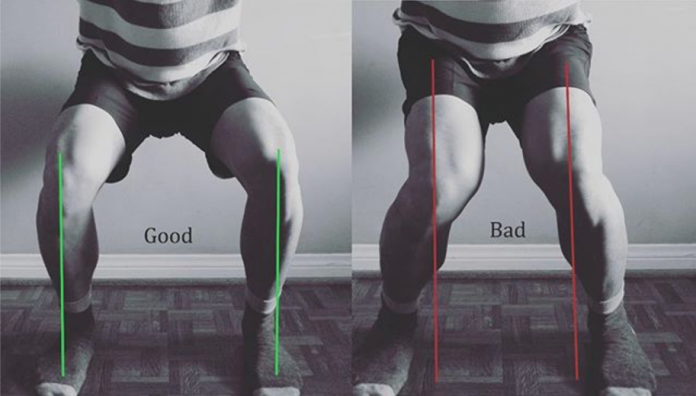
Which makes quite a bit of sense — up to 70% of non-contact ACL injuries occur when an athlete is cutting or changing direction. But that just makes it doubly as important to recognize and correct improper mechanics during said movements (especially as you’re going through rehab).
Common Issue #4: Lack of Confidence
Each of these issues are entirely common on their own… but they often come paired with a general lack of confidence. Which is entirely understandable; it’s natural to fear “undoing” all the time and work you’ve put into your recovery.
But, it’s also vital that you acknowledge that it’s precisely because of your work that you’re likely able to take on more than you realize.
Of course, you’ll want to be sure you have the data and know-how to do everything safely; but if you’ve been sticking to your training and adhering to your physical therapist’s guidance, your body’s a lot more prepared to handle the demands of single-leg workouts. (After all, these movements and mechanics have been a part of your rehabilitation for months now!)
Unlearning that lack of confidence can certainly be a tough mental hurdle to work through. But remember: it’s far from permanent! The more you learn and practice proper form and execution, the more your mindset will adapt to recognizing your rebuilt strength, coordination, and agility. You’re well on your way to getting back to your usual activity, and no uncertainty is going to keep you down!
Goals for Month 7 of ACL Rehabilitation
Now that you’ve passed the halfway mark of your rehab timeline, it’s important to really hone in on any remaining deficiencies in your form — especially for single-leg activities.
Although you’ll eventually get to a point where your training focuses on physical activity with both legs, it’s vital to train each leg individually. It’s all about balance, and we don’t mean that because it’s on just one leg. Focusing on one leg at a time ensures that your injured leg can handle the demands of exercise just as your uninjured leg does.
So, here are the goals you can keep in mind as you train your way through this next month:
- Control pelvic drop — practice weightbearing, single-leg exercises to get your body familiar with keeping a level pelvis. Otherwise, your body will begin to compensate with lateral trunk lean to keep you from toppling over when on one leg.
- Improve your shock absorption — the key to this single-leg work is to include more of a plyometric element and to focus on coordination throughout your lower extremity. (Make sure both legs can handle forces equally!)
- Normalize quadriceps and gluteus maximus/medius strength — as per usual, those lower extremity muscles need some good ol’ fashioned strength work. By this point, your strength improvements should be close to or at optimal levels, so it’s more about maintaining consistency than making significant strength gains.
- Perform multi-direction agility drills — similarly, you’re going to continue your agility work the more you progress through your single-leg exercises. You’re now likely going to perform these drills at 50-75% of your maximum speed.
- Perform variable practice with distracting stimuli — this is a continuation from last month, where you’re learning how to practice quick and accurate sports movements with the added element of external stimuli. (This includes throwing a ball while jumping, catching a ball while decelerating or cutting, and changing direction at the last minute.)

Who’s Ready for Month 8?
And there you have it: month 7!
You may have noticed that many of your exercises won’t be drastically different from what you’ve already been doing… But! They have a different purpose this time around.
At the very start of your rehab, your exercises and training are loosely guided by how much pain you’re experiencing; your physical therapist will frequently ask you if or when certain movements hurt and how much. However, by month 7, your training requires an entirely different set of questions:
Does this movement feel as strong as your uninjured side? Do you feel confident performing this specific drill? Do you feel weakness anywhere while practicing sports movements?
Are you worried you’re going to get hurt again?
It’s understandable to still feel hesitant or uncertain, but remember: you’ve made immense progress since day one. Be honest with where you’re struggling (both physically and mentally), and trust that you and your physical therapist will design a definitive program that will yield significant progress towards a full recovery.
Then, take a deep breath, and keep your head up as you progress into month 8.

